The notion of physician-assisted passing has ignited a profound ethical discourse on a global scale. At its core lies the poignant query: ought individuals, confronted by insurmountable anguish brought on by terminal afflictions, be granted the prerogative to conclude their own existence with the aid of a healthcare expert?
The idea of autonomy is crucial to the conversation. People who support physician-assisted dying argue that they have the right to make decisions about their own existence, including when and how they die away. This viewpoint values the autonomy and standard of living of patients, highlighting the fact that certain fatal illnesses can cause prolonged and degrading suffering. Advocates claim that by giving patients the option of a peaceful death, their autonomy is respected and upheld.
On the other hand, some who oppose physician assistance in dying express concerns about the potential for involuntary euthanasia and the denigration of human life. They highlight that the use of life termination by medical professionals runs counter to the fundamental medical precept of “do no harm.” This viewpoint often results from religious or philosophical beliefs that view life as sacred and untouchable. Sceptics are concerned that legalising assisted suicide could damage the doctor-patient relationship and erode community safeguards against abuse.
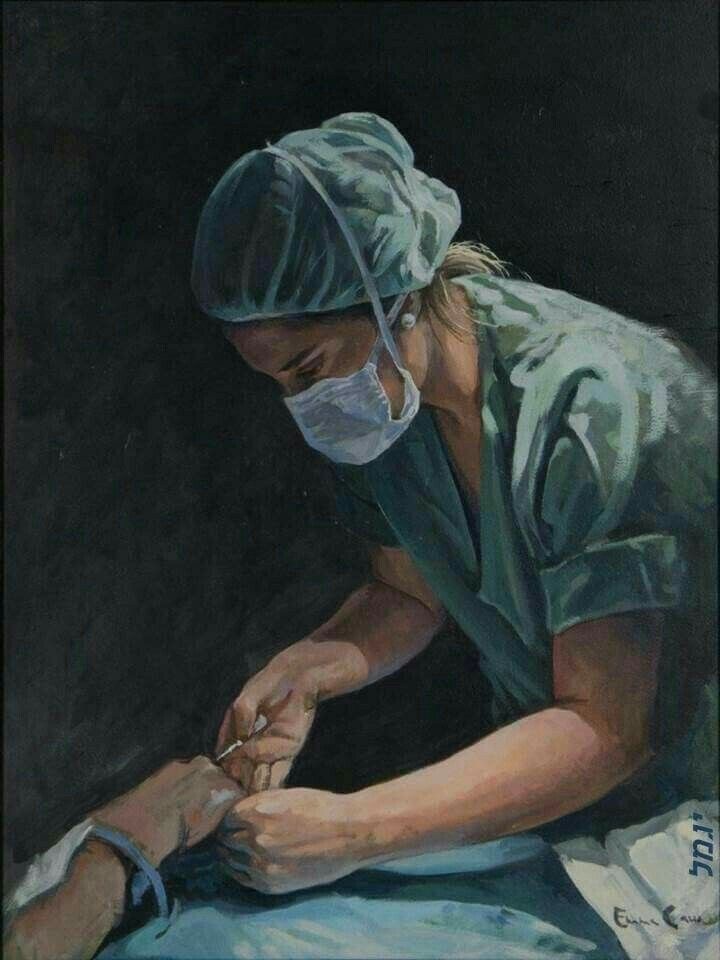
There is a split on this issue within the medical profession itself. While some doctors support assisted suicide as a compassionate act, others believe it conflicts with their duty to treat patients. The psychological effects on themselves and their coworkers are a worry for those who reject the practise. It can be emotionally upsetting to carry the ethical burden of helping a patient die away, which can lead to concerns about burnout in the workplace and moral ambiguity.
The discussion is significantly shaped by the existing legal frameworks as well. The Netherlands, Belgium, and a few states in the United States and Australia are among the jurisdictions that have legalised physician-assisted suicide. These states have also passed strict regulations to ensure a careful and secure decision-making process. In order to prevent rash decisions, waiting periods and assessments by different medical professionals are frequently required. But detractors claim that these protections might not be perfect, allowing open for the possibility of force or manipulation.
Ethical concerns also extend to vulnerable people, particularly the elderly and crippled. Concerns have been raised that these populations may face pressure to choose assisted suicide as a result of societal biases or economic considerations. The need to avoid any appearance of force becomes critical in order to protect these people from potential marginalisation or manipulation into decisions that do not truly reflect their desires.

Furthermore, debates about physician-assisted suicide act as a springboard for more in-depth discussions about palliative care and end-of-life care. Opponents argue that improving palliative care choices would ease suffering without resorting to assisted suicide. Increased spending in pain treatment, psychological support, and hospice care, they argue, could provide patients with a dignified and comfortable death.
The ethical issues surrounding physician-assisted suicide are complex and multifaceted. The interaction of human autonomy, medical ethics, and societal safeguards emphasises the importance of thoughtful and well-informed conversations on this subject. Striking a balance between giving patients the right to a peaceful exit and protecting against potential abuses remains a difficult task. In the face of evolving legal and medical perspectives, it is critical to prioritise a respectful discourse that recognises the many perspectives of patients, medical practitioners, ethicists, and society at large.
Sources
- https://onlinedegrees.bradley.edu/blog/what-ethical-issues-can-arise-with-end-of-life-care/#:~:text=Known%20as%20one%20of%20the,or%20respecting%20the%20patient’s%20wishes.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4934577/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4934577/
- https://journals.sagepub.com/doi/full/10.1177/20503121211000918
- https://www.forbes.com/sites/avivahwittenbergcox/2022/10/22/a-designed-death–where–when-the-world-allows-it/?sh=2840e0777b3d#:~:text=Before%201997%2C%20only%20Switzerland%20permitted,2021%20and%20Australia%20(2022).